Testosterone, an essential hormone the testicles produce, plays a pivotal role in men’s health. Understanding the function of the testicles and the hormones they produce is vital to appreciating their impact on various aspects of male well-being, including sexual health, physical strength, and emotional balance.
Primary Function:
The testicles within the scrotum are crucial organs in the male reproductive system. They are responsible for producing sperm, which is essential for reproduction.
Hormonal Role:
Beyond sperm production, the testicles are the primary source of testosterone in males. This hormone is vital for developing male sex characteristics, including muscle mass, bone density, and body hair.
Testosterone and Men’s Health:
Broad Impact:
Testosterone’s influence extends beyond the reproductive system. It affects mood, energy levels, libido, and overall physical health.
Age-Related Changes:
As men age, testosterone levels naturally decline, which can impact several areas of health, including sexual function and mood.
Testosterone Levels and Erectile Dysfunction:
Correlation with ED:
Testosterone plays a significant role in erectile function. While not the only factor, low testosterone levels (hypogonadism) can contribute to erectile dysfunction (ED).
The Link:
ED can stem from various causes, both physical and psychological. The relationship between testosterone levels and ED is complex and multifactorial. Low testosterone can lead to reduced libido, which in turn can affect erectile function.
The testicles and the testosterone they produce are integral to men’s health, with a direct impact on physical, sexual, and emotional well-being.
The Testicles
The testicles are critical organs in the male reproductive system, not only for their role in sperm production but also as the primary site for testosterone synthesis.
Testicular Anatomy:
The testicles are oval-shaped organs housed within the scrotum, a pouch of skin hanging below the penis. This external location is crucial for temperature regulation, as sperm production requires a temperature slightly lower than the body’s core.
Each testicle comprises coiled tubes called seminiferous tubules, where sperm are produced. These tubules are surrounded by a structure known as the epididymis, where sperm mature and are stored.
The testicles are supplied with blood by the testicular arteries and have a complex network of nerves, making them sensitive organs.
Role in the Male Reproductive System:
One of the primary functions of the testicles is spermatogenesis – the production of sperm. This process is continuous and takes about 64 days to complete.
The testicles are also responsible for producing male hormones, especially testosterone. The hypothalamus and pituitary gland regulate this production by releasing hormones such as LH (Luteinizing Hormone) and FSH (Follicle-Stimulating Hormone).
Testosterone Production Process:
The hypothalamic-pituitary-gonadal axis regulates the production of testosterone. The hypothalamus releases GnRH (Gonadotropin-releasing Hormone), which stimulates the pituitary gland to produce LH and FSH.
LH stimulates the Leydig cells in the connective tissue between the seminiferous tubules to produce testosterone.
Testosterone is crucial for the development of male secondary sexual characteristics, such as increased muscle mass, deeper voice, and facial hair. It also plays a vital role in sexual function, libido, and overall well-being.
Testosterone
Testosterone, often characterised as the quintessential male hormone, plays a pivotal role in various aspects of men’s health beyond its well-known functions in reproduction. This hormone, predominantly produced in the testicles, influences multiple physiological and psychological processes.
Testosterone’s Role:
Testosterone is crucial for developing male secondary sexual characteristics during puberty, including the growth of facial and body hair, deepening of the voice, and changes in body structure.
Testosterone significantly contributes to muscle growth and strength. It aids in synthesising muscle protein, increasing muscle mass and maintaining muscle strength and endurance.
This hormone plays a vital role in bone health. It helps maintain bone density, reducing the risk of osteoporosis and bone fractures, particularly in older men.
Psychological and Emotional Influence:
Testosterone can have a profound impact on mood. Low levels of this hormone have been linked to mood swings, irritability, and depression.
Emerging research suggests that testosterone may influence cognitive functions, including memory and concentration.
Testosterone is closely linked to sexual desire. A decrease in testosterone levels can lead to a reduction in libido. It can be a contributing factor in erectile dysfunction (ED).
Testosterone Throughout the Lifespan:
Testosterone levels naturally decline with age, typically beginning in a man’s 30s and continuing progressively. This decline can affect various aspects of health, from physical stamina to sexual function.
Lifestyle factors such as diet, physical activity, stress, and sleep can influence testosterone levels. Healthy lifestyle choices can help in maintaining optimal testosterone levels.
Testosterone and Erectile Dysfunction
The intricate relationship between testosterone levels and erectile function is a crucial area of focus in understanding and treating erectile dysfunction (ED). Testosterone, while not the sole factor, plays a significant role in maintaining erectile health.
Impact of Testosterone on Erectile Function:
Testosterone is integral to sexual desire or libido. A reduction in testosterone levels can lead to a decreased interest in sexual activity, which can indirectly affect the ability to achieve and maintain an erection.
Testosterone helps in the dilation of blood vessels, facilitating the blood flow necessary for an erection. Low levels of this hormone can lead to difficulties in achieving sufficient penile rigidity.
Testosterone aids in the synthesis of nitric oxide. This molecule plays a crucial role in the erectile process by relaxing the smooth muscles of the penis and allowing blood inflow.
Low Testosterone (Hypogonadism) and ED:
Hypogonadism, a condition characterised by low testosterone levels, can be a contributing factor to ED. It can be classified as primary (resulting from testicular issues) or secondary (due to hypothalamic or pituitary disorders).
Men with hypogonadism may experience other symptoms, such as fatigue, muscle weakness, decreased bone mass, and mood changes, alongside ED.
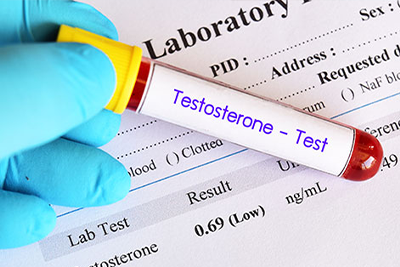
Diagnosing Testosterone Deficiency:
Diagnosing low testosterone involves a combination of blood tests to measure hormone levels, along with a review of symptoms and medical history.
Treatment for ED related to low testosterone often involves testosterone replacement therapy (TRT), alongside lifestyle modifications and other interventions targeted at improving erectile function.
Addressing Testosterone Imbalances:
Addressing lifestyle factors such as diet, exercise, sleep, and stress management can positively affect testosterone levels and erectile health.
For men with ED and low testosterone, a comprehensive treatment plan that addresses both hormonal imbalances and other factors contributing to ED is crucial for effective management.
Causes of Low Testosterone in Men
Testosterone levels in men can be influenced by various factors, ranging from natural ageing to specific lifestyle choices and health conditions.
Common Causes of Reduced Testosterone Production:
Hypogonadism is where the testes produce few or no hormones and can be present from birth or develop later in life due to infection or injury.
Disorders of the pituitary gland or hypothalamus, which controls hormone production, can lead to decreased testosterone levels.
Conditions like type 2 diabetes, obesity, liver or kidney disease, and HIV/AIDS can negatively impact testosterone production.
Certain medications, including opioid pain medications, hormones used to treat prostate cancer, and steroids, can affect testosterone levels.
Age-Related Changes in Testosterone Levels:
Testosterone levels naturally decline as men age, typically around 30 to 40. This decline is gradual, at about 1% to 2% per year.
Some men experience a more significant drop in testosterone levels, leading to symptoms of late-onset hypogonadism, especially in their 60s and beyond.
Lifestyle and Health Factors Affecting Testosterone:
Excess body fat, particularly abdominal fat, can disrupt the balance of hormones, including testosterone.
A diet lacking in essential nutrients and a sedentary lifestyle can contribute to lower testosterone levels.
Abuse of alcohol and drugs can negatively impact testosterone production.
Chronic stress and inadequate sleep can lead to hormonal imbalances, including reduced testosterone levels.
Exposure to certain chemicals and toxins, such as endocrine disruptors in some plastics, can affect testosterone production.
Recognising Symptoms of Low Testosterone
Low testosterone in men can manifest in various physical, emotional, and cognitive symptoms. Recognising these signs is crucial for timely intervention and treatment.
Physical Symptoms of Low Testosterone:
One of the most noticeable symptoms is a decreased interest in sexual activity.
Difficulty in achieving or maintaining an erection can be linked to low testosterone levels.
Testosterone plays a role in building muscle, so reduced levels may lead to decreased muscle mass.
Men with low testosterone might notice an increase in body fat, sometimes with enlarged breast tissue.
Lower testosterone can weaken bones, increasing the risk of osteoporosis and fractures.
A general feeling of tiredness and a lack of energy can be a symptom of low testosterone.
Emotional and Cognitive Symptoms:
Men with low testosterone may experience mood swings, irritability, or depression.
Some men might feel demotivated, less confident, or generally less happy.
Issues with memory, concentration, and decision-making can also be symptoms.
Timely Recognition and Consultation:
Recognising these symptoms is critical as they can significantly impact a man’s quality of life, relationships, and mental health.
If you notice symptoms of low testosterone, it’s essential to consult a healthcare provider. They can conduct appropriate tests to confirm the diagnosis and identify underlying causes.
Early detection and treatment of low testosterone can prevent more severe health issues, improve symptoms, and enhance overall health and well-being.
Since these symptoms can also indicate other health conditions, a comprehensive evaluation is crucial to rule out other potential causes.
Diagnosing Testosterone Levels
Accurately measuring and interpreting testosterone levels is essential for diagnosing testosterone deficiency in men. In the UK, specific guidelines and procedures are followed to ensure a reliable diagnosis.
Measuring Testosterone Levels:
The most common method for assessing testosterone levels is through a blood test. Blood is typically drawn in the morning when testosterone levels are at their highest. Total testosterone levels are measured, including free (active) and bound testosterone (inactive).
Testosterone levels are measured in nanomoles per litre (nmol/L) in the UK. A normal range can vary but is typically around 10-30 nmol/L. Levels below the lower limit are generally considered indicative of testosterone deficiency.
It’s important to note that testosterone levels can fluctuate due to various factors like time of day, age, and overall health.
Alongside blood tests, a comprehensive clinical assessment is crucial. This includes evaluating symptoms like low libido, fatigue, mood changes, and ED.
The NHS recommends more than one blood test to confirm low testosterone levels, as levels can vary from day to day and even within the same day.
Testosterone levels naturally decline, so age-specific reference ranges are often considered in diagnosing testosterone deficiency.
Other health conditions like obesity, diabetes, and certain medications can affect testosterone levels. The diagnosis considers these factors to ensure it’s not a secondary effect of another condition.
Given that symptoms of low testosterone can overlap with other health issues, accurate diagnosis is crucial to avoid misdiagnosis and ensure appropriate treatment. Determining the correct cause of symptoms guides the choice of treatment—for example, lifestyle changes, testosterone replacement therapy, or treating underlying conditions.
Treating Low Testosterone and Managing ED
Addressing low testosterone levels is a crucial aspect of managing erectile dysfunction (ED) in men, where hormonal imbalance is a contributing factor. Testosterone replacement therapy (TRT) and other treatment options can significantly improve symptoms of both low testosterone and ED. However, weighing the risks and benefits of these treatments is essential.
Testosterone Replacement Therapy (TRT):
TRT is designed to bring testosterone levels back to normal in men diagnosed with hypogonadism. It can be administered through gels, patches, injections, or subcutaneous pellets.
By normalising testosterone levels, TRT can improve libido and erectile function in men whose ED is linked to low testosterone.
Testosterone levels are monitored during TRT to ensure efficacy and safety. Dosages may be adjusted based on response and side effects.
Other Treatment Options for ED Related to Low Testosterone:
PDE5 Inhibitors can be effective in treating ED, including in men with low testosterone.
Addressing lifestyle factors such as diet, exercise, and stress management can improve overall health and potentially increase testosterone levels.
Psychological support, including sex therapy or counselling, can be beneficial, especially if stress, anxiety, or relationship issues contribute to ED.
Risks and Benefits of TRT:
Benefits of TRT include improved libido, mood, energy levels, muscle mass, and bone density. It can also enhance the quality of life for men with significantly low testosterone levels.
Potential risks of TRT include an increased risk of cardiovascular events, sleep apnea, and prostate issues. It can also cause skin reactions, infertility, and a decrease in testicle size.
TRT is not suitable for everyone. Men with prostate or breast cancer, severe urinary symptoms, or heart failure may need to avoid TRT.
Men must discuss TRT’s potential risks and benefits with their healthcare provider, considering their health profile and specific needs.
Lifestyle Factors in Boosting Testosterone and ED Management
Lifestyle choices play a significant role in managing testosterone levels and erectile dysfunction (ED). Combining diet, exercise, stress management, and sleep quality can boost testosterone levels and improve erectile function.
Dietary Considerations:
A diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain optimal testosterone levels. These foods provide essential vitamins, minerals, and antioxidants that support hormonal balance.
Incorporating healthy fats, such as omega-3 fatty acids found in fish and nuts, is beneficial for testosterone production.
Limiting processed foods, mainly those high in sugars and unhealthy fats, can prevent testosterone levels and overall health fluctuations.
Exercise’s Role in Enhancing Testosterone Levels:
Regular exercise, particularly weight and high-intensity interval training (HIIT), has increased testosterone levels.
While exercise is beneficial, excessive physical stress from overtraining can negatively impact testosterone levels. Finding a balanced exercise routine is vital.
Stress Reduction and Its Impact:
Chronic stress elevates cortisol levels, which can inversely affect testosterone. Techniques like mindfulness, meditation, yoga, or other relaxation methods can help manage stress.
Addressing mental health issues, such as anxiety and depression, through counselling or therapy can positively impact testosterone levels and ED.
Sleep Quality and Testosterone Levels:
Quality sleep is crucial for testosterone production. Poor or inadequate sleep can significantly reduce testosterone levels.
Establishing a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants before bedtime can improve sleep quality.
Lifestyle Modifications for ED Management:
Smoking and excessive alcohol consumption can worsen ED. Reducing or quitting these habits can have a positive effect on erectile function.
Being overweight or obese can contribute to lower testosterone levels and ED. Weight management through diet and exercise is beneficial.
Preventive Measures for Maintaining Healthy Testosterone Levels
Maintaining healthy testosterone levels is crucial for men’s health overall. Proactive and preventive measures, including daily habits and regular health check-ups, are significant in preserving testicular health and sustaining optimal testosterone levels.
Daily Habits and Practices:
A diet rich in whole foods, low in processed sugars and unhealthy fats, and balanced in proteins, fats, and carbohydrates supports hormonal health.
Regular physical activity, including strength training and cardiovascular exercises, can help maintain healthy testosterone levels.
Maintaining a healthy weight is crucial. Obesity can lead to lower testosterone levels and associated health issues.
Managing stress through relaxation techniques, mindfulness, and adequate leisure time can help regulate cortisol levels, supporting healthy testosterone production.
Limiting alcohol intake and avoiding tobacco and recreational drugs can positively impact testosterone levels.
Ensuring sufficient quality sleep each night is essential, as testosterone production is closely linked to sleep patterns.
Regular Health Check-Ups and Screenings:
Regular health check-ups can help monitor overall health, including factors affecting testosterone levels, such as weight, blood pressure, and cholesterol levels.
Regular testicular self-exams and professional examinations can help detect issues like lumps or changes in the testicles that might indicate health concerns affecting testosterone levels.
Men experiencing symptoms of low testosterone or those with risk factors should consider hormonal screenings to check testosterone levels.
Conditions like diabetes, metabolic syndrome, and cardiovascular diseases can affect testosterone levels. Monitoring and managing these conditions are essential for maintaining hormonal balance.
Proactive Lifestyle Adjustments:
Continuously assessing and adjusting lifestyle factors such as diet, exercise, and stress is crucial in maintaining healthy testosterone levels.
Consulting with healthcare professionals for personalised advice on testosterone maintenance and overall health is beneficial.
In conclusion, preserving testicular health and maintaining healthy testosterone levels involves a combination of daily health practices, regular medical check-ups, and proactive lifestyle adjustments.
Related Articles
- What Your Testicles Are Telling You
- A Fresh Approach to Tackling ED with P-Shot
- Causes of Erectile Dysfunction in the UK
- Understanding the Signs and Symptoms of Low Testosterone Every Man Should Know About
- The Potential of Testosterone Replacement Therapy: Benefits, Risks, and Myths