Plantar fasciitis (Fashee-EYE-Tiss) is a prevalent cause of heel discomfort. Plantar fasciitis was once assumed to be an inflammatory process, we know now that it is a disorder of progressive degeneration in the plantar fascia causes a thickening of the fiber. The fibrous tissues, known as fascia, run from your heel bone (calcaneus) to the tips of your toe bones (metatarsals). Together, they form the plantar surface of your foot. It’s a repetitive stress injury caused by putting too much pressure on the plantar fascia for it to handle. The plantar fascia’s stress threshold differs between individuals. Up to 10% of the population suffers from plantar fasciitis, making it the most frequent cause of heel discomfort.
Plantar fasciitis is the root cause of most cases of heel discomfort. This condition is most common among middle-aged males and females (40-60), while it affects people of all ages and is especially prevalent among athletes. It is believed that the repetitive motions involved in these activities produce the plantar fascia injury seen in these athletes.
Causes of Plantar Fasciitis
Plantar fasciitis has multiple, separate causes. The underlying aetiology of the disorder is unknown. The proposed causes can be categorized into two groups:
Inherent:
- Excessive inward pronation of the foot (increased pronation)
- Very flat feet (flat feet)
- Extremely arched feet
- Overly-tight calf muscles or Achilles’ tendons
- Hamstring strain
- Reduced range of motion in the ankle joint
- Excessive body fat
External:
- Jobs that need constant movement. Plantar fasciitis is common among people who spend their days walking or standing on hard surfaces, such as factory employees, teachers, chefs, nurses, and cleaners.
- Unsuitable footwear
Symptoms of Plantar Fasciitis
Pain described as “sharp” or “stabbing,” specifically in the area of the heel bone, is diagnostic of plantar fasciitis, which occurs when the plantar fascia runs along the bottom of the foot and becomes inflamed and irritated. Plantar fasciitis symptoms seem to be at their worst in the morning after waking up. The discomfort may go away for a while, only to return after extended periods of standing or walking.
Post-static dyskinesia is characterized by pain upon standing after a prolonged period of rest. The sensation has been likened to walking barefoot on marble and is typically described as intense and stabbing. The plantar fascia’s continual attachment to the foot’s arch is a common source of pain in certain people, but it can also spread laterally across the sole.
Diagnosis of Plantar Fasciitis
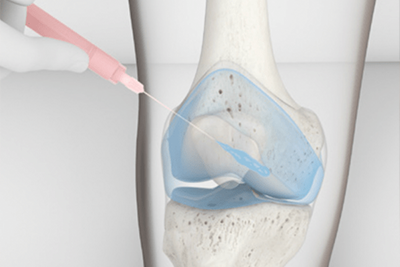
In most cases, a podiatrist or other appropriately trained medical expert will diagnose plantar fasciitis based on a patient’s history that is consistent with the characteristic symptoms of plantar fasciitis. Ultrasound and magnetic resonance imaging (MRI) are two types of diagnostic imaging that are sometimes utilized but not always necessary to confirm a diagnosis.
Diagnostic imaging is also helpful for ruling out alternate diagnoses, like radiculopathy (backache), bone oedema (swelling), plantar fascia rupture, stress fracture, inflammatory illnesses, etc.
Why Does My Foot Hurt?
Plantar fasciitis develops when this brutal band of ligamentous connective tissue, which extends from the heel to the foot ball, becomes inflamed. This sturdy and taut tissue helps support the foot’s arch. When you walk or run, it’s also a powerful weight transmitter over your foot. As a result, there is a great deal of strain on this tissue. Plantar fasciitis occurs when the arch of the foot’s connective tissue is damaged from repeated stress beyond its tolerance level, leading to thickening and degeneration. One’s plantar fascia may have become overstretched for a variety of reasons. It could be a combination of pronating feet and tight calf muscles (roll-in). For some, the problem could be caused by standing for extended periods while wearing inappropriate footwear. The plantar fascia is subject to stress from a variety of sources.
Can Plantar Fasciitis be Treated?
In a word, yes. Yet, there is no one-size-fits-all remedy for plantar fasciitis. The most crucial step is determining what caused it in the first place, as causes vary from person to person. There are several things you can do:
- Rest and ease up on the things that aggravate the discomfort
- Application of ice for pain reduction
- As a form of alternative medicine, massage has been shown to have positive effects
- Donning a night splint
- Conducting a regular regimen of strengthening and stretching exercises
- Proper support footwear
- Using orthotic devices for the feet (insoles)
- Shockwave therapy
This is by no means an exhaustive list.
Should I See a Doctor?
Some people can treat plantar fasciitis at home, but if the pain persists beyond three weeks, it’s best to see a doctor. Orthotic inserts, foot tape, cortisone shots, night splints, anti-inflammatory medicines, and physical therapy are some treatments a sports podiatrist could offer. Checking with your doctor or chiropractor will also allow for diagnostic procedures like X-rays and another imaging testing to confirm that plantar fasciitis is the root cause of your foot pain.
How Long Will Discomfort Last?
This is a complex subject because many things affect a person’s ability to heal from an injury, including their general health and the presence or absence of specific medical disorders. These include, but are not limited to, diabetes, immune deficiency, poor blood flow, and so on. Most cases of plantar fasciitis result from cumulative microtrauma. How effectively you respond to treatment is also affected by how long you’ve had the ailment. We know that diseases that last longer than six months are harder to repair and less responsive to traditional treatment. Therefore, your prognosis improves the sooner you begin treatment.
Why Does Treatment Sometimes Not Work?
The majority of cases of chronic pain can be treated without surgery. Statistics consistently show that nonsurgical treatment is successful in 90% of cases. Patients usually respond positively to plantar fasciitis treatment if the underlying problems are treated. Most treatment failures occur because of unsuitable recommendations or because patients do not follow doctors’ orders, such as by not using the right shoes or not doing exercises as directed. Unfortunately, chronic plantar fasciitis often does not respond to treatment (having the condition for over six months). Scar tissue can accumulate and cause degeneration of the plantar fascia in long-term occurrences. This renders traditional treatments less effective and increases the difficulty of treating the problem. Extra-corporeal shockwave therapy is one treatment option for chronic conditions since it stimulates the body’s natural healing response. In a subsequent piece, we’ll delve deeper into this potential course of action. Misdiagnosis, in which another form of heel pain is mistaken for plantar fasciitis, is another common reason treatment doesn’t work.
How Can I Prevent Pain Returning?
Since muscle tightness is a common contributor to plantar fasciitis, you must keep your newly found flexibility. To accomplish this, you should engage in flexion and extension once every few days or whenever you feel your muscles tightening. Keeping the newfound adaptability will lessen the likelihood that you’ll have to start over.
Wearing the right shoes is just as crucial. This is not to say that you must always wear shoes that provide adequate arch support. It simply means that the risk of recurrence will grow if you spend all of your time in uncomfortable shoes.
Can I Still Run?
Rest is always the first step in relieving pain, no matter your treatment plan. Running and step aerobics, which causes pain from the repetitive pounding of the feet on hard surfaces, may need to be reduced or stopped altogether, depending on the individual’s circumstances. Consult a medical professional if you have any doubts about whether a particular exercise is appropriate for you.
What Precautions Can I Take?
If you are susceptible to plantar fasciitis, it is crucial to take precautions even if you have never had it before or are just now feeling better. Get shoes with good arch support and heel cushioning from a specialised retailer. Preventing the foot issue can be done by doing exercises that strengthen the legs and ankles and stretching the plantar fascia and Achilles tendon. Always warm up before working out, and don’t suddenly increase your intensity. A runner shouldn’t add over 10 percent to their weekly distance.
Related Articles
- Plantar Fasciitis or Achilles Tendonitis
- Exercises for Plantar Fasciitis
- Treatment of Plantar Fasciitis using Shockwave Therapy
- Shockwave Therapy For Heel Pain
- 7 Sporting Injuries Your Chiropractor Can Help With