Do you suffer from Pelvic Pain?
If you are currently experiencing Pelvic Floor Pain, you know how distressing it can be. However, you are not alone. It can affect both men and women, starting suddenly, and unlike a sore arm or a painful lower back, it doesn’t go away quickly; left untreated, it may get worse and become chronic.
What does Pelvic floor pain feel like? The symptoms of pelvic floor pain are various. They can be described as burning, tingling, shooting, crushing, and ‘electric shocks.’ These can be felt in the perineum (the area between the testicles and anus) and genitals, groin area, and pubic region. The pain can also be felt in the coccyx with referred pain to the calf, foot, and toes. Other symptoms can include sexual dysfunction, difficulties with urination and bowel emptying with or without pain, and reduced awareness of defecation. It can also feel like the bladder has not emptied, and the patient feels like they have to ‘go again’ immediately after leaving the toilet.
The pain often interrupts sleep, and the patient can find it challenging to get into a comfortable position. The pain can be continuous or intermittent without any relief affecting the quality of everyday life.
Sitting can be extremely painful, also. It can feel like ‘sitting on hot coals’ or ‘sitting on a golf ball’. Some patients can only sit by wrapping cold packs in tea towels on a soft cushion. The harder the chair, the more painful it is to sit. Patients often spend most of the day standing, trying to avoid sitting as much as possible, or if they have to sit for work, they prefer soft seating and standing frequently (every 10-15 mins) to relieve pain. Sitting on a hard office chair or park bench can aggravate or be impossible. Doughnut cushions can alleviate some but could make things worse for others. Sitting for long periods can cause increased ‘crushing’ and numbness around the sit bones and buttocks.
The pain can be felt along the path of the pudendal nerve, which starts at the bottom of the spine and goes into the anus, perineum, prostate, bladder, testes, and penis, which is highly unpleasant. The burning pain often worsens after urinating and bowel movements. Patients with pre-existing IBS, anal fissures, and haemorrhoids can suffer considerably.
Patients try to avoid long car journeys as much as possible, and going out to a social event such as a restaurant, cinema, or theatre can seem terrifying. Understandably this chronic pelvic pain can have a devastating effect on mental health and general self-confidence.
Treatments:
Your first thought will probably be, ‘Just stop the pain or reduce it, please,’ when visiting your GP, which is perfectly understandable. Your GP will probably give you some specialist medication for nerve pain. You may be taking Paracetamol or Ibuprofen already before you visit your GP.
If you are suffering from burning pain, you can buy several cold packs, keep them in the freezer, and use them as much as you need. Cold packs straight out of the freezer can cause a ‘cold burn’, so give them a few minutes to reach room temperature and place them on a soft cushion with tea towels covering them. If you feel too cold, add more layers of tea towels. If you can’t feel enough cooling – remove some tea towels.
Physiotherapy is a critical factor in aiding your recovery. Your pelvic floor physiotherapist will give you a printout of various pelvic floor exercises you can do from home daily; they will also show you how to do each exercise to ensure you are doing them correctly. A good quality yoga mat is essential. Some exercises can be done on your bed before sleep to calm the whole body and pelvic floor muscles. Learning the correct breathing technique of ‘breathing into the tummy’ rather than the chest is also crucial. ‘Breathing into the tummy’ and training your brain to learn the idea of ‘sending the breath to the perineum’ relaxes the pelvic floor muscles. When the human body is in constant pain, everything naturally tightens up and causes further emotional and physical stress creating a vicious cycle. Breathing is your best friend to help relax the body, and it is 100% side effect free. Your physiotherapist will do manual manipulation to relax the pelvic floor muscles and pudendal nerve, some of which may include anal work, as that is the best path to access the pudendal nerve and pelvic muscles; this is not painful and far less uncomfortable than a prostate exam. Some physiotherapists are also trained in acupuncture, which many patients have found helpful.
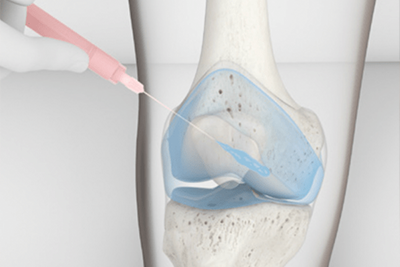
Your physiotherapist may also be able to refer you to the ‘Pain Clinic’ at your local hospital, where you will see a Pain Consultant. This doctor specialises in helping patients suffering from chronic pain anywhere in the body. They can administer various treatments, including a pudendal nerve block, ganglion block, epidural block, and pulse radio frequency to help numb the pain. This could give you some lasting pain relief.
Focused Shockwave Therapy is another option; it is a safe and effective method of treating pelvic muscle and nerve pain. Your pelvic floor physiotherapist or specialist chiropractor may have access to a shock wave machine. This treatment causes minor trauma to the area, which can activate the body’s healing system to ‘kick in’ and start repairing the damaged pelvic floor. This is typically done throughout six weekly sessions and is a non-invasive procedure. The shockwave therapy can feel slightly uncomfortable, a bit like acupuncture; your practitioner will lower or increase the intensity of the shockwave machine to meet your needs.
Constipation is your worst enemy when it comes to pelvic floor health. Straining when going to the toilet puts additional pressure on the pelvic floor. You may feel a sharp increase in pain after an episode of constipation. Eat plenty of fruits and vegetables to avoid constipation (aim to get five or more daily). Walking and gentle cardio is an excellent ways to stabilise your pelvic floor. A healthy diet and cardio exercise are also very beneficial.
Pelvic floor pain can be extremely mentally and physically draining, so seeking help from a physiatrist or physiologist can be very helpful and is nothing to be ashamed of. Cognitive Behavioural Therapy, or ‘CBT’ is a type of talking therapy that teaches you coping skills for dealing with different problems. Family members or work colleagues may find it difficult to understand what you are going through and may even make unhelpful comments such as, ‘It is all in your head.’ Chronic pain can devastate your mental health, so seeking help from a qualified practitioner is crucial to your recovery.
Related Articles
- Shockwave Therapy FAQs
- Penis Pain and Pelvic PT
- Shockwave Therapy as an Aid to Physical Rehabilitation
- Are There Any Side Effects of Shockwave Therapy
- Shockwave Therapy as a Treatment for Erectile Dysfunction