Osteoarthritis (OA) of the knee is widespread, affecting millions, particularly older adults. As the most common form of arthritis, OA is a degenerative joint disease that gradually breaks down the cartilage in the knee, leading to pain, stiffness, and reduced mobility. These symptoms can make everyday activities—like walking, climbing stairs, or even standing for extended periods—challenging and painful, ultimately diminishing a person’s quality of life.
Although knee osteoarthritis is often associated with ageing, it can affect individuals of various ages due to joint injuries, obesity, or genetic predisposition. With the progressive condition, managing symptoms early on is crucial to prevent further deterioration.
Osteoarthritis in the Knee
Osteoarthritis (OA) is a chronic, degenerative joint disease characterised by the gradual breakdown of cartilage, the smooth tissue that cushions the ends of bones in joints. In healthy joints, this cartilage allows bones to move smoothly against each other, but in OA, the cartilage becomes thinner and less effective. Over time, as the cartilage deteriorates, bones begin to rub directly against each other, causing pain, swelling, stiffness, and a reduced range of motion. In some cases, small bony growths, known as osteophytes, may also develop around the joint, contributing to discomfort and reduced mobility.
While osteoarthritis can affect any joint, knee osteoarthritis is prevalent due to the significant strain on this weight-bearing joint. Every step, jump, or movement involving the knee applies force to the joint, which, over time, can contribute to cartilage breakdown, particularly in overweight individuals who are physically active in high-impact sports or have previously injured the joint.
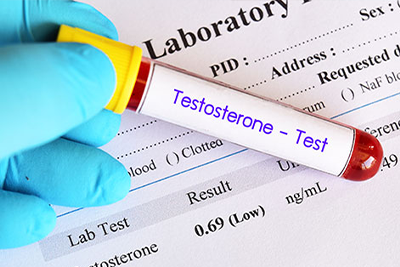
In the UK, osteoarthritis is the most prevalent form of arthritis, affecting millions of people, particularly those over the age of 45. However, OA is not exclusive to older adults. Younger people may also develop knee OA due to various factors, including previous knee injuries, genetic predisposition, or repetitive stress on the joint from occupations or activities that require prolonged kneeling, squatting, or heavy lifting.
Symptoms of Knee Osteoarthritis
Knee osteoarthritis typically develops gradually, and its symptoms can vary from mild discomfort to more severe pain and mobility issues. The early stages of OA often present subtle signs that may be mistaken for normal ageing or overuse. However, recognising these symptoms early is crucial for effective management and to slow disease progression.
One of the first symptoms many people notice is joint stiffness, particularly in the morning or after periods of inactivity, such as sitting for long durations. This stiffness usually eases with movement but can return after resting or at the end of the day. As osteoarthritis progresses, the knee joint may become more painful during movement, especially during activities that put pressure on the knee, such as walking, climbing stairs, or standing for long periods.
Another common symptom is swelling and inflammation around the knee. This occurs due to the body’s response to the cartilage wearing down and increased bone friction. The swelling can range from mild to more pronounced, often leading to a feeling of warmth in the joint.
Many people with OA in the knee report a grating or crunching sensation, also called crepitus, when moving the joint. This can occur as the cartilage breaks down, allowing the bones to rub against each other. In more advanced cases, this can cause significant discomfort and limit normal movement.
As OA worsens, the knee joint’s range of motion and flexibility often reduces. Simple tasks like bending the knee, walking, or getting up from a seated position can become difficult. This reduced mobility can lead to further weakening of the muscles around the knee, exacerbating the condition.
Lastly, people with knee osteoarthritis may experience difficulty performing everyday tasks like walking, climbing stairs, or standing up. This can significantly impact the quality of life, making it essential to seek medical advice early. Timely intervention with lifestyle changes, exercises, and treatments can help manage symptoms and prevent further deterioration.
Non-Surgical Management of OA Knee Pain
Managing knee osteoarthritis doesn’t always require surgical intervention. Several non-surgical treatments have effectively reduced pain, enhanced mobility, and improved overall quality of life. These approaches focus on lifestyle changes, physical therapy, and medications, offering long-term relief without more invasive procedures.
-
Exercise and Physical Therapy
Exercise plays a vital role in managing OA knee pain. Regular physical activity strengthens the muscles surrounding the knee joint, providing better support and reducing stress on the joint itself. Low-impact exercises, such as swimming, cycling, and walking, are particularly effective as they place minimal strain on the knees while improving flexibility and endurance. Working with a physiotherapist can help you develop a personalised exercise plan tailored to your needs. These exercises will enhance flexibility, build strength, and improve balance, contributing to better knee function and reduced discomfort.
-
Weight Management
For overweight individuals, losing even a small amount of weight can significantly reduce the pressure on the knee joint. Excess weight strains the knees, accelerating cartilage wear and intensifying pain. Research suggests that for every pound lost, there is a corresponding reduction in knee joint stress. Consequently, weight loss not only alleviates pain but also helps slow the progression of osteoarthritis. NHS guidelines strongly advocate weight management as a central component of OA treatment, making it a lifestyle change for many patients.
-
Pain Relief Medications
Pain relief medications can provide short-term relief for osteoarthritis symptoms. Over-the-counter options such as paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are often recommended to manage pain and reduce inflammation. For those seeking a targeted approach, topical treatments containing NSAIDs, available in gels or creams, can offer localised pain relief with fewer systemic side effects compared to oral medications. This is especially useful for individuals who may have underlying health conditions or are sensitive to the side effects of oral pain relievers.
-
Assistive Devices
Various assistive devices can also help alleviate the strain on the knee joint, improving mobility and reducing discomfort. Walking aids such as canes or walking sticks provide extra support, taking pressure off the knee during movement. Similarly, knee braces can offer additional stability, particularly during physical activities. Orthotic insoles, designed to correct foot alignment, can redistribute weight more evenly, reducing the pressure on the knee and potentially easing pain. These devices are often recommended with other therapies to optimise movement and pain relief.
Cingal® Option for Managing OA Knee Pain
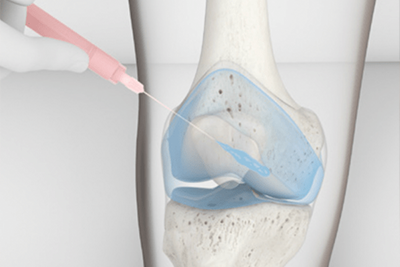
For individuals seeking more advanced treatment options for knee osteoarthritis, Cingal®, now available at the Vale Health Clinic in Tunbridge Wells, offers an innovative solution. Cingal® is a unique injectable treatment combining hyaluronic acid with a steroid, providing immediate and long-lasting relief from osteoarthritis pain. This dual-action injection is designed to reduce knee pain, improve mobility, and delay the need for surgical interventions like knee replacement.
-
Cingal®
Cingal® is injected directly into the knee joint, serving two critical functions. The hyaluronic acid component acts as a lubricant and shock absorber, enhancing the joint’s ability to glide smoothly and reducing bone friction. This helps alleviate pain caused by the loss of cartilage typical in osteoarthritis. The steroid component of the injection works quickly to reduce inflammation in the joint, offering almost immediate pain relief. Together, these components provide both short-term and long-term benefits, with many patients experiencing pain relief that lasts up to six months or more after treatment.
Cingal® is particularly beneficial for individuals with moderate to severe knee osteoarthritis who have not responded adequately to other non-surgical treatments, such as oral medications, physiotherapy, or lifestyle modifications. It is an ideal option for patients looking to delay or avoid surgery, such as knee replacement, by managing their pain and improving mobility through less invasive means. Cingal® can be used alongside other management strategies, including exercise routines, weight management, and assistive devices, to maximise overall joint function.
-
Cingal® at Vale Health Clinic
At the Vale Health Clinic, located in Tunbridge Wells, specialists in osteoarthritis management are available to assess whether Cingal® is the right option for your condition. The clinic offers a comprehensive evaluation to determine the most effective treatment, ensuring that Cingal® is combined with a tailored plan to manage knee osteoarthritis effectively. Its convenient location makes it accessible for patients in Kent and the surrounding areas.
When Surgery Becomes Necessary
While non-surgical treatments for knee osteoarthritis can be highly effective for many individuals, there are cases where surgical intervention becomes necessary. If symptoms worsen or non-invasive options, such as medications, physical therapy, or injections, no longer provide adequate relief, knee surgery may be considered. This is typically the path for those with severe osteoarthritis, where the joint damage is extensive, and daily activities are severely impacted by pain and reduced mobility.
Knee replacement surgery (arthroplasty) is the most common surgical treatment for advanced knee osteoarthritis. During the procedure, damaged parts of the knee joint are replaced with artificial metal and plastic components. The aim is to restore function, relieve pain, and improve the patient’s overall quality of life. Advances in surgical techniques and materials have significantly improved knee replacements’ success rate and durability, with many patients experiencing substantial long-term benefits.
However, surgery is generally considered a last resort. Healthcare providers will often explore all non-surgical options first to manage symptoms. Surgery involves risks, such as infection or blood clots, and requires significant recovery. Therefore, it’s essential to have a thorough discussion with your doctor about the timing and necessity of surgery if your knee osteoarthritis continues to worsen. The decision to proceed with knee replacement will depend on factors such as the extent of joint damage, your age, activity level, and overall health.
For those experiencing severe pain that limits everyday activities, a well-timed surgical intervention can lead to significant improvements in both function and comfort, allowing for a return to a more active lifestyle.
Living Well with Osteoarthritis
Although osteoarthritis is a chronic condition, the proper lifestyle and treatment plan can significantly improve your ability to manage pain, maintain mobility, and continue leading an active life. Take a proactive approach with knee osteoarthritis, combining medical treatments with everyday habits that promote joint health and overall well-being.
One of the most impactful lifestyle changes you can make is to stay active. Regular physical activity, especially low-impact exercises like swimming, walking, or cycling, can help keep your muscles strong and your joints flexible. Strengthening the muscles around the knee can reduce strain on the joint, which may alleviate pain and slow the progression of osteoarthritis. A physiotherapist can guide you through personalised exercises designed to improve strength, flexibility, and balance, crucial to staying mobile with OA.
In addition to staying active, eating a balanced diet is crucial in managing osteoarthritis. Maintaining a healthy weight reduces the pressure on your knees, easing pain and reducing the risk of further joint damage. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support joint health. Foods high in omega-3 fatty acids, such as oily fish, may also help reduce joint inflammation.
Using joint-protection strategies is another essential aspect of living well with osteoarthritis. This includes techniques like pacing yourself during activities, using assistive devices when necessary, and avoiding movements that strain your knees unnecessarily. Simple changes in how you move and perform daily tasks can significantly reduce pain and preserve your joint health.
The NHS and local health services offer access to support groups and patient education programmes for additional support. These resources can provide valuable information on managing osteoarthritis and offer a sense of community for those with the condition. Connecting with others with similar experiences can help you stay motivated and informed while providing emotional support.
By combining medical treatments such as Cingal® with lifestyle changes and the support of healthcare professionals, you can manage knee osteoarthritis effectively and continue to live a full, active life.
Related Articles
- Knee Osteoarthritis (OA) Symptoms and Treatment
- Understanding Osteoarthritis of the Knee
- Osteoarthritis Management and Self Care
- Benefits of Hyaluronic Acid Injections for Osteoarthritis
- Osteoarthritis and Arthritis, Similar But Very Different