Erectile dysfunction (ED), clinically defined as the persistent inability to achieve or maintain an erection sufficient for satisfactory sexual performance, remains a significant medical concern for a substantial portion of the male population in the United Kingdom.
As a testament to its pervasive nature, recent estimates suggest that approximately 4.3 million men in the UK experience ED, underlining its position as a significant public health issue. This figure translates to roughly 1 in 5 men aged 40 and over contending with this condition. The consequences of ED span beyond the physical, often permeating psychological, emotional, and relational, underscoring the importance of comprehensive understanding and proactive medical intervention. As we delve deeper into the intricate landscape of ED, the relevance of lifestyle factors in exacerbating or mitigating its occurrence becomes increasingly evident.
The Escalating Challenge of ED with Age
A defining characteristic of erectile dysfunction (ED) is its association with age. As men progress through the stages of life, the prevalence of ED sees a marked incline. Clinical epidemiological data furnishes some clarity on this trajectory: Within the age bracket of 40 to 70 years, 40% of men grapple with varying degrees of ED. This percentage sees a notable spike as we consider the older demographic, with approximately 70% of men aged 70 and above reporting the condition.
Furthermore, although ED can manifest at various stages of an individual’s life, it’s worth highlighting that the mean age of onset is calculated to be 45 years old. This statistic underscores the notion that midlife can serve as a critical inflection point for many men, where physiological changes coupled with lifestyle factors might converge to precipitate the onset of ED. Such trends in age-related prevalence serve as a poignant reminder of the necessity for early intervention, appropriate medical consultation, and proactive health management to mitigate the challenges posed by ED in later life stages.
Lifestyle Factors Amplifying the Risk of ED
Weight and Obesity
A burgeoning body of evidence underscores the linkage between excess body weight and the increased susceptibility to erectile dysfunction (ED). Overweight and obese men are found to be at a heightened risk of ED when juxtaposed against their counterparts with healthy weight ranges. The root of this association can be traced back to the physiological repercussions of obesity. Excess fatty tissue can instigate a series of vascular and metabolic alterations, notably endothelial dysfunction and reduced nitric oxide availability. These changes compromise blood flow, a fundamental requirement for achieving and maintaining an erection. Moreover, obesity can precipitate hypertension, dyslipidaemia, and insulin resistance, further amplifying the risk.
Sedentary Lifestyle
Physical inactivity, a hallmark of a sedentary lifestyle, is emerging as a potent predictor of ED. A lack of regular exercise or physical exertion can foster a cascade of cardiovascular and metabolic derangements, thereby augmenting the ED risk. Men leading primarily sedentary lives exhibit a diminished vascular health profile, potentially impairing penile blood flow. Encouragingly, interventional studies have indicated that augmenting physical activity levels can alleviate and reverse ED in some cases.
Smoking
The pernicious effects of tobacco consumption on erectile health are well-documented. Statistically, men who smoke are approximately twice as susceptible to ED as non-smokers. The primary etiological agent behind this association is the vascular damage inflicted by cigarette smoke. Tobacco compounds, notably nicotine, engender vasoconstriction and endothelial dysfunction, impeding the hemodynamic imperative for an erection. Furthermore, chronic smoking exacerbates atherosclerotic changes, narrowing blood vessels and further challenging erectile function.
High Blood Pressure and Cholesterol
Hypertension, or high blood pressure, carries a substantial clinical weight in the context of ED, with afflicted men bearing a risk three times greater than those with normotensive readings. Similarly, elevated cholesterol levels double the risk of ED. Both these conditions, individually and synergistically, jeopardise vascular integrity. Impaired arterial elasticity and vessel occlusion, common sequelae of these conditions, can significantly compromise penile blood inflow, an indispensable factor for achieving erections.
Diabetes
Diabetes mellitus, characterised by chronic hyperglycaemia, is intrinsically linked to ED. Men with diabetes are approximately twice as likely to experience ED than those without this metabolic disorder. The bidirectional relationship between diabetes and ED stems from multiple avenues, including vascular damage, autonomic neuropathy, and endothelial dysfunction. Chronic elevated blood sugar levels wreak havoc on blood vessels and nerves, both integral to the erectile process. Furthermore, the metabolic perturbations associated with diabetes, like dyslipidaemia, augment the risk profile.
Other Contributing Factors
Mental Health
The intricate interplay between psychological well-being and erectile function is increasingly gaining clinical recognition. Two prominent psychological conditions, depression and anxiety, have been identified as significant risk factors for the onset and perpetuation of erectile dysfunction (ED). The aetiology of this association is multifaceted. Psychogenic ED, predominantly stemming from these mental health conditions, underscores the disruption of the cerebral components imperative for initiating and maintaining an erection. Neurotransmitter imbalances, commonly seen in depression and anxiety, can hinder the neurological pathways facilitating erectile function. Furthermore, the emotional and cognitive disturbances associated with these conditions—such as low self-esteem, performance anxiety, and relationship stresses—can exacerbate the problem, creating a cyclical pattern of psychological distress and impaired erectile function.
Medications
Several therapeutic agents, while beneficial for their primary indications, have been identified as potential culprits in the development or worsening of ED. Due to their pharmacological actions, these medications can interfere with the hemodynamic, neurological, or hormonal processes essential for normal erectile function. Notable drug classes implicated include certain antihypertensives (like beta-blockers), antidepressants (specifically SSRIs), antipsychotics, and some diuretics. It’s pivotal for clinicians and patients alike to be aware of these potential side effects, considering alternative medications or dosage adjustments when ED becomes a concern.
Family History
The genetic landscape of ED, though not entirely elucidated, suggests a hereditary component to the condition. Men with a familial history of ED, particularly among first-degree relatives, exhibit an elevated risk of developing the condition. Several genetic markers and polymorphisms are being researched for their potential role in this heredity. While lifestyle and environmental factors undoubtedly play a considerable part, a genetic predisposition could potentiate the risk, underscoring the importance of a comprehensive family medical history during clinical evaluations of ED.
While modifiable lifestyle factors significantly influence the risk and severity of ED, intrinsic factors like mental health, medication use, and genetics also wield substantial influence. A holistic understanding of these factors ensures a more comprehensive and practical approach to diagnosing, managing, and preventing ED.
Proactive Lifestyle Changes to Combat ED
Dietary Recommendations
Dietary habits can play a pivotal role in modulating the risk and severity of erectile dysfunction (ED). Embracing a heart-healthy diet promotes cardiovascular wellness and concurrently supports erectile function. Foods rich in omega-3 fatty acids, such as fatty fish (e.g., salmon, mackerel, and sardines), flaxseeds, and walnuts, aid in reducing systemic inflammation and improving vascular integrity. Likewise, a diet abundant in fruits, vegetables, whole grains, and lean proteins can help maintain optimal blood pressure and cholesterol levels, which are crucial for erectile health. Conversely, limiting the intake of saturated fats, trans fats, and excess sugars can prevent conditions predisposing one to ED.
Exercise and Physical Activity
Regular physical activity offers manifold benefits, including alleviating ED risk. Cardiovascular exercises like walking, jogging, cycling, and swimming can enhance blood circulation and vascular health, benefiting erectile function. Strength training, in moderation, aids in testosterone production—a hormone integral to libido and erectile health. Furthermore, pelvic floor exercises, often termed Kegel exercises for men, have improved the muscles’ strength in the erectile and ejaculatory process. A consistent routine comprising 150 minutes of moderate-intensity exercise weekly is generally advocated for overall health and ED prevention.
Stress Management Techniques
Acute and chronic stress can be a formidable antagonist to erectile function due to its disruptive influence on hormonal balance and neural pathways. Incorporating stress-reducing techniques can provide respite from the psychological impediments to ED. Breathing exercises, notably diaphragmatic and paced breathing, can alleviate acute episodes of anxiety. Mindfulness practices, encompassing meditation and progressive muscle relaxation, foster present-moment awareness, curtailing the negative spiral of performance anxiety. Lastly, guided imagery and biofeedback can offer individuals tools to self-regulate their physiological responses to stress.
Avoidance of Tobacco and Limiting Alcohol
Tobacco cessation is paramount for those seeking to mitigate ED risk. As detailed earlier, the vascular complications wrought by smoking are detrimental to erectile health. Individuals wanting to stop smoking can get help with pharmacotherapeutic aids, counselling, and support groups, all of which have demonstrated efficacy in tobacco cessation. Regarding alcohol, while moderate consumption might not pose significant risks, chronic and excessive intake can impair testosterone production and neural function. Men should adhere to recommended guidelines, which typically advocate for no more than 14 units of alcohol spread evenly across a week.
In conclusion, adopting proactive lifestyle modifications can be a potent strategy for preventing and managing ED. These changes, while benefiting erectile health specifically, also foster holistic well-being, underscoring their multifaceted relevance.
Related Articles
- Causes of Erectile Dysfunction in the UK
- Prevalence of Erectile Dysfunction in the UK
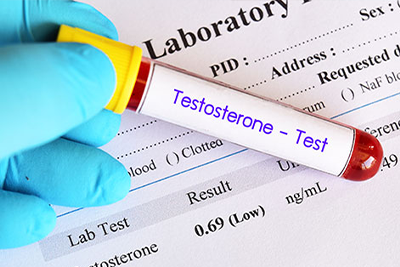
- Understanding the Link Between Testosterone and Erectile Dysfunction
- Erectile Dysfunction and Underlying Health Conditions
- Psychological Aspects of Erectile Dysfunction