Erectile dysfunction (ED), a medical term often shrouded in silence and misconception, pertains to the recurrent inability of an individual to achieve or sustain an erection sufficient for satisfactory sexual activity. While transient episodes can be commonplace, rooted in factors like stress or fatigue, a persistent pattern warrants medical attention.
In the UK, the gravity of this condition is underscored by its prevalence: it’s estimated that ED affects around 1 in 5 men aged 40 and over, culminating in an estimated 4.3 million men grappling with this condition. This data does more than just highlight the issue’s magnitude; it beckons an in-depth understanding of the causative underpinnings.
For many, ED isn’t an isolated disorder but a symptom of underlying systemic conditions. Delving deeper into these coexisting health concerns not only unravels the comprehensive nature of ED but also empowers affected individuals and healthcare professionals alike to instigate holistic interventions. Recognising the multifaceted causes of ED and its associations is thus paramount for effective diagnosis, management, and, potentially, prevention.
The Cardiovascular Connection
Erectile dysfunction (ED) and cardiovascular health are inexorably linked, echoing the overarching narrative of vascular integrity and function. The penile erection is, at its core, a vascular event, necessitating a harmonious interplay of blood vessels to facilitate blood influx and retention within the corpora cavernosa. Any impediment in this vascular orchestration can culminate in ED.
In the UK, a significant proportion of men with ED are found to have concurrent cardiovascular ailments. Research indicates that among men diagnosed with ED, approximately 40% also exhibit symptoms of cardiovascular diseases. The pathophysiology binding these conditions primarily revolves around arterial health.
Atherosclerosis, a condition where arteries narrow and harden due to plaque build-up, impairs blood flow. While this compromised circulation can manifest as coronary artery disease affecting the heart, it surfaces as ED when impacting the penile arteries. Similarly, endothelial dysfunction, a scenario where the inner lining of the blood vessels doesn’t function optimally, leads to reduced nitric oxide production, a molecule essential for achieving erections.
In short, the same arterial conditions that heighten the risk of heart attacks, strokes, and other cardiovascular diseases can directly influence a man’s ability to achieve and maintain an erection. Recognising ED as potentially more than just a sexual health issue but a barometer of one’s cardiovascular health underscores the importance of holistic evaluation and care.
Endocrinological Implications
The endocrine system, an intricate network of glands producing hormones, is indispensable in regulating many physiological processes, including sexual function. When these hormonal symphonies falter, the repercussions can be felt in various health aspects, notably erectile function.
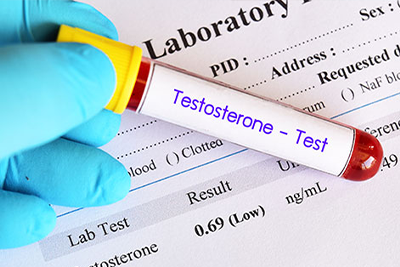
Central to this discussion is testosterone, the primary male sex hormone. Testosterone modulates libido, muscle mass, bone density, and erectile function. Due to age or pathological conditions, its declining levels can lead to diminished sexual desire and compromised erectile function. While the relationship between low testosterone and ED isn’t linear—many men with reduced testosterone levels don’t always suffer from ED—it’s undeniable that a deficiency can exacerbate erectile difficulties.
In the UK, it’s estimated that around 2% of men exhibit overt symptoms of testosterone deficiency. Of this subset, a significant portion report ED as a primary concern. However, it’s crucial to understand that while testosterone replacement therapy might benefit some men, it isn’t a panacea for all cases of ED. The decision to treat must always be rooted in comprehensive clinical evaluation.
Endocrine-related ED extends beyond just testosterone. While less common, hyperthyroidism, hypothyroidism, and hyperprolactinemia can manifest as ED. Moreover, the systemic implications of diabetes, which will be discussed in subsequent sections, are deeply intertwined with endocrinological dysfunctions leading to erectile issues.
Neurological Associations
The intricate dance of achieving and maintaining an erection is not solely a vascular event but a symphony directed by the nervous system. The central (brain and spinal cord) and peripheral nervous systems play pivotal roles in the erectile process, orchestrating signals that result in the physical manifestation of arousal.
This neural network’s core is the events that lead to an erection. It starts with sensory or mental stimuli that trigger nerve signals from the brain, descending the spinal cord and culminating in the release of neurotransmitters in the penile tissues. This cascade of events leads to the dilation of penile arteries, the influx of blood, and consequent erection.
However, disruptions in this neural pathway, often stemming from neurological disorders, can impede this process. For instance:
Parkinson’s disease: Characterised by the death of nerve cells in the brain, this disorder can hinder the brain’s ability to communicate sexual arousal signals, leading to ED.
Multiple sclerosis (MS): A condition wherein the immune system mistakenly attacks the protective covering of nerve fibres. MS can interrupt the transmission of nerve signals responsible for erections.
Other conditions: Spinal cord injuries, stroke, Alzheimer’s disease, and even some surgeries related to prostate treatments can damage nerves and subsequently influence erectile function.
In the UK, the prevalence of neurologically induced ED remains a concern. For instance, among men diagnosed with Parkinson’s disease, roughly 40% report symptoms of ED. Similarly, around 50% of men with multiple sclerosis experience some degree of erectile dysfunction. These figures serve as a testament to the integral role of the nervous system in erectile health.
Understanding the neurological basis of ED widens our perspective and offers avenues for targeted therapeutic interventions, ultimately driving towards a more tailored approach to patient care.
The Dual Threat from Diabetes
Diabetes mellitus is one of the leading chronic conditions intimately linked with erectile dysfunction (ED). This relationship isn’t just unidirectional—diabetes can lead to ED, and conversely, ED can be an early indicator of undiagnosed diabetes.
In the UK, the interlink between diabetes and ED is starkly evident. Studies suggest that over 50% of men with diabetes will experience some degree of erectile dysfunction within a decade of their diagnosis. Such data is particularly alarming, considering that over 4 million individuals are diagnosed with diabetes in the UK.
Delving into the mechanistic underpinnings of this association reveals multiple factors at play:
Vascular Damage: Diabetes, mainly when poorly managed, results in chronic hyperglycaemia. This elevated blood sugar can damage blood vessels, impairing their ability to dilate correctly—a process fundamental for achieving erections.
Neuropathy: Chronic diabetes can lead to diabetic neuropathy, wherein prolonged high blood sugar levels damage the nerves. Since nerve signals are instrumental in achieving erections, their compromise can lead directly to ED.
Impaired Nitric Oxide Synthesis: Nitric oxide (NO) acts as a vasodilator, facilitating the influx of blood into the penile tissues. Diabetes can inhibit the synthesis and function of NO, thereby hindering the process of erection.
Beyond these mechanistic pathways, diabetes also brings associated conditions such as cardiovascular diseases, which compound the risk of ED.
Psychological Underpinnings
Erectile dysfunction (ED), often perceived as a physiological ailment, has deep-rooted psychological dimensions. The intricate interplay between the mind and the body means that emotional and cognitive states can significantly influence erectile function.
The connection between mental health and ED is evident in the prevalence of psychological conditions among ED sufferers. In the UK, studies have shown that approximately 20% of ED cases are primarily due to psychological factors, with depression and anxiety being the most common culprits.
Depression: The heavy weight of chronic sadness, low mood, and lack of interest characteristic of depression can significantly impact sexual desire and function. Neurochemically, depression is associated with an imbalance in serotonin and dopamine levels—neurotransmitters vital for mood regulation and sexual response. The frequent use of certain antidepressants can further exacerbate ED, creating a vicious cycle where treatment for one condition might aggravate the other.
Anxiety: The anticipatory anxiety about sexual performance can be a self-fulfilling prophecy. Men who experience a single episode of ED often fear recurring attacks, leading to ‘performance anxiety’. This heightened alertness can release adrenaline, a hormone that contracts blood vessels, inhibiting the necessary blood flow for an erection.
Beyond these specific conditions, other psychological stressors like relationship problems, trauma, and chronic stress can also precipitate or worsen ED.
Understanding the neurochemical imbalances and their impact provides a nuanced perspective. For instance, serotonin, often termed the ‘feel good’ neurotransmitter, plays a pivotal role in mood regulation. However, excessive levels can inhibit sexual desire and arousal. Similarly, dopamine, vital for pleasure and reward, influences sexual desire. An imbalance in these neurotransmitters, often seen in depression and anxiety, can directly impact erectile health.
Medication-Induced ED
While medications are designed to ameliorate symptoms or cure disorders, they sometimes come with unintended side effects—one of which, for specific drug classes, is erectile dysfunction (ED). Understanding the scope and specifics of medication-induced ED becomes paramount, especially in the UK, where prescription drug use is prevalent.
A telling statistic underscores this concern: up to 25% of ED cases in the UK might be attributed to medication side effects. These cases highlight the importance of routinely reviewing and evaluating the medication list of men presenting with ED.
The following are some of the commonly prescribed drugs in the UK with potential links to ED:
Antihypertensives: Medications to control high blood pressure, such as beta-blockers and diuretics, can result in ED. The mechanism primarily revolves around their ability to decrease blood flow to the penis, making erections difficult to achieve and maintain.
SSRIs (Selective Serotonin Reuptake Inhibitors): These antidepressants, which increase serotonin levels to counteract depressive symptoms, can dampen sexual desire and impair erectile and ejaculatory functions.
Antiandrogens: Used primarily in prostate cancer treatment, these medications inhibit testosterone activity, leading to decreased sexual desire and ED.
H2 Antagonists: Drugs like ranitidine, used for acid reflux, have been associated with ED, although the exact mechanism remains elusive.
Others: This category includes drugs such as antipsychotics, antiarrhythmics, and even some antihistamines, all of which have been associated with ED to varying degrees.
The challenge often lies in discerning whether the ED results from the medication itself, the condition it’s treating, or a combination of both. For instance, while antihypertensives can cause ED, hypertension is a risk factor for ED. This intertwined relationship necessitates a collaborative approach between healthcare professionals and patients, where potential risks are weighed against therapeutic benefits.
Renal Health and ED
The kidneys, vital organs for maintaining the body’s internal equilibrium, also play an unassuming role in maintaining erectile function. However, various kidney diseases can upset this balance, leading to erectile dysfunction (ED).
In the UK, the convergence of renal health and ED is pronounced. Data reveals that approximately 50% of men with chronic kidney disease (CKD) stages 3-5 experience ED. This alarming statistic underscores the need to consider renal health when assessing erectile function, especially given the rising prevalence of kidney ailments in the UK population.
The pathophysiology connecting kidney diseases to ED is multifaceted:
Hormonal Shifts: Kidneys play a vital role in regulating hormones, including testosterone and erythropoietin. CKD often leads to a decrease in these hormones, reducing sexual desire and contributing to ED.
Vascular Complications: Kidney diseases, particularly CKD, are frequently accompanied by other vascular conditions, like hypertension and atherosclerosis, which can reduce blood flow to the penis and thus lead to ED.
Medication Implications: Many medications prescribed to manage kidney diseases, like antihypertensives, can further increase the risk of ED.
Nerve Function: Uremia, a severe manifestation of kidney disease, can impact nerve function, further exacerbating ED problems.
Psychological Factors: Chronic kidney disease and the need for dialysis can also lead to depression, anxiety, and reduced self-esteem, all of which can contribute to ED.
Furthermore, the medications used to treat high blood pressure in the context of kidney disease might exacerbate ED, as highlighted earlier. It is also noteworthy that men on dialysis have reported a higher prevalence of ED, possibly due to the combined effect of the disease, medications, and psychological factors.
Proactive Monitoring and Collaborative Care
Erectile dysfunction (ED) serves as more than a marker of men’s reproductive health — it frequently signals deeper, systemic health issues. Addressing ED, therefore, demands an integrative and proactive approach centred on holistic health and backed by a multidisciplinary team.
Beyond its impact on quality of life and relationships, ED serves as a barometer of overall health. Conditions such as cardiovascular disease, diabetes, and renal health issues, among others, intertwine with ED, making it essential for healthcare providers to take a comprehensive view. Addressing the root causes not only helps in managing ED but also improves overall health outcomes.
Given the ties between ED and systemic health conditions, at-risk individuals, especially those with a family history or exhibiting early signs of diseases like hypertension or diabetes, should undergo regular health screenings. This proactive monitoring can lead to early detection and timely interventions, potentially preventing the onset of ED.
Cardiovascular Check-ups: Due to the vascular nature of ED, regular heart health check-ups, including cholesterol levels and blood pressure readings, become crucial.
Endocrinological Assessments: Monitoring testosterone levels and other hormonal markers can pinpoint imbalances that might contribute to ED.
Mental Health Evaluations: Given the psychological dimensions of ED, routine mental health assessments can detect underlying issues like depression or anxiety that may be exacerbating or causing ED.
Managing and potentially reversing ED is often beyond the purview of a single healthcare provider depending on underlying conditions.
Concluding, it’s evident that a siloed approach to ED is insufficient. As understanding its intricacies and links to broader health concerns grows, proactive monitoring and a collaborative care model emerge as the gold standard for its management. By fostering an environment where open communication thrives, and holistic care is prioritised, it becomes possible to manage ED and enhance overall health and quality of life.
Related Articles
- Prevalence of Erectile Dysfunction in the UK
- Causes of Erectile Dysfunction in the UK
- Lifestyle Factors Impacting Erectile Dysfunction
- Understanding Testosterone Deficiency and the Role of Hormone Replacement
- Psychological Aspects of Erectile Dysfunction