Diabetes and erectile dysfunction (ED) are two prevalent conditions that significantly impact men’s health in the UK. Diabetes, a chronic condition marked by elevated levels of blood sugar, affects millions of individuals, influencing various aspects of their health and well-being. Erectile dysfunction, characterised by the inability to achieve or maintain an erection sufficient for satisfactory sexual performance, similarly affects a considerable proportion of the male population, especially those living with diabetes. The intersection of these two conditions presents unique challenges and underscores the need for comprehensive understanding and management.
The relationship between diabetes and ED is complex and multifaceted. Diabetes can lead to ED through a variety of mechanisms, including damage to blood vessels and nerves, which are crucial for achieving and maintaining an erection. The prevalence of ED among men with diabetes is alarmingly high, making it a significant concern that necessitates attention and action.
The purpose of this article is twofold: to illuminate the link between diabetes and erectile dysfunction and to dispel common myths surrounding these conditions. Misinformation and misconceptions about diabetes and ED can hinder effective management and treatment, leaving many men without the support and care they need. By providing accurate information and highlighting the importance of managing diabetes and ED, this article aims to empower men to take control of their health, seek appropriate medical care, and improve their quality of life.
Diabetes
Diabetes mellitus, commonly called diabetes, is a chronic condition characterised by high blood glucose (sugar) levels. It occurs when the body cannot effectively use or produce insulin, a hormone that regulates blood sugar. Understanding the types of diabetes, their causes, symptoms, and long-term implications is essential for managing the condition and preventing complications, including erectile dysfunction (ED).
Types of Diabetes
Type 1 Diabetes:
This autoimmune condition results in the body’s immune system attacking and destroying the insulin-producing cells in the pancreas. It typically manifests in childhood or young adulthood. Individuals with Type 1 diabetes require lifelong insulin therapy to manage their condition.
Type 2 Diabetes:
Far more common than Type 1, Type 2 diabetes develops when the body becomes resistant to insulin or when the pancreas cannot produce enough insulin. It is strongly linked to lifestyle factors, including obesity, physical inactivity, and poor diet, although genetics also play a role.
Causes and Symptoms
Causes:
While the exact cause of Type 1 diabetes is unknown, genetic and environmental factors are believed to contribute. Type 2 diabetes is more closely associated with lifestyle factors, such as excess weight and sedentary behaviour.
Symptoms:
Common symptoms of both types include frequent urination, excessive thirst, fatigue, blurred vision, and unexplained weight loss. Type 2 diabetes symptoms can be subtle and develop slowly over time.
Long-term Health Implications
Complications:
Uncontrolled diabetes can lead to severe health complications, including cardiovascular disease, nerve damage (neuropathy), kidney damage (nephropathy), eye damage (retinopathy), and increased risk of infections.
Impact on Sexual Health:
Diabetes can specifically impact sexual health by causing ED in men. High blood sugar levels can damage the blood vessels and nerves essential for an erection, making diabetes a significant risk factor for ED.
Diabetes in the UK
Diabetes is a growing concern in the UK, with millions of people diagnosed with the condition. The prevalence of diabetes has been increasing steadily, highlighting a significant public health challenge.
The rising prevalence of diabetes places a substantial burden on the UK healthcare system, necessitating effective prevention, early diagnosis, and comprehensive management strategies. Efforts are focused on addressing the lifestyle factors contributing to Type 2 diabetes and providing support for individuals living with Type 1 diabetes.
Link Between Diabetes and Erectile Dysfunction
The intricate relationship between diabetes and erectile dysfunction (ED) is grounded in the physiological repercussions of prolonged high blood sugar levels, which can significantly impair vascular health and nerve function.
Physiological Effects
Vascular Damage:
Chronic high blood sugar levels, a hallmark of diabetes, can lead to damage in the blood vessels, including those that supply blood to the penis. This damage impairs the vessels’ ability to dilate and constrict properly, a critical process in achieving and maintaining an erection. The resulting compromised blood flow is a direct pathway to erectile dysfunction.
Nerve Damage (Neuropathy):
Diabetes can also cause neuropathy or damage to the nerves due to high glucose levels in the blood over time. Since the process of achieving an erection requires precise communication between the brain, nervous system, and penile tissue, neuropathy can disrupt these signals, leading to difficulties in attaining or maintaining an erection.
Endothelial Dysfunction:
Beyond the mechanical aspects of blood flow, diabetes is associated with endothelial dysfunction, where the inner lining of blood vessels fails to function normally. This condition further hampers the production of nitric oxide, a molecule essential for vasodilation during an erection.
Increased Risk of ED Among Men with Diabetes
Prevalence Studies:
Research consistently shows that men with diabetes are at a significantly increased risk of developing ED. Studies indicate that men with diabetes are three times more likely to experience ED compared to men without diabetes.
Temporal Relationship:
The risk of ED increases with the duration of diabetes. Men who have had diabetes for ten years or more are at a higher risk of ED, emphasising the impact of long-term glucose control on sexual function.
Impact of Glycemic Control:
Several studies have found a direct correlation between glycemic control and the severity of ED. Poor glycemic control exacerbates the risk and severity of erectile dysfunction, while good management of blood sugar levels can mitigate this risk to some extent.
Comprehensive Reviews:
Meta-analyses and systematic reviews of the literature further solidify the connection between diabetes and ED, providing a robust evidence base that underscores the need for targeted interventions to manage ED in this population.
Symptoms and Early Detection of ED in Diabetic Men
Erectile dysfunction (ED) in the context of diabetes often manifests subtly, gradually intensifying as both conditions progress. Recognising the symptoms early and understanding their implications is crucial for diabetic men to seek timely intervention, potentially mitigating the severity of ED and improving overall outcomes.
Symptoms of ED in Diabetic Men
Difficulty Achieving an Erection:
One of the earliest signs of ED in diabetic men is the increased difficulty in achieving an erection sufficient for sexual intercourse. This may initially occur only occasionally but can become more frequent over time.
Trouble Maintaining an Erection:
Even if an erection is achieved, maintaining it throughout sexual activity can become challenging. This symptom, like difficulty in attaining an erection, may worsen as diabetes progresses.
Reduced Sexual Desire:
While not directly a symptom of ED, a decrease in libido or sexual desire can accompany ED in diabetic men. This reduction can stem from the psychological impact of ED, as well as from diabetes-related hormonal changes.
Inconsistent Erectile Function:
Variability in erectile function, where a man experiences normal erectile function one day and difficulty the next, can also be a sign of ED in the context of diabetes.
Early Detection
Preventing Progression:
Early detection of ED can halt its progression and, in some cases, reverse its effects. Recognising symptoms as soon as they appear increases the likelihood of successful management through lifestyle modifications, medical treatment, or both.
Identifying Underlying Health Issues:
Since ED can be an early warning sign of vascular problems and neuropathy associated with poorly controlled diabetes, early detection offers a critical window for addressing these underlying health issues. Improving diabetes management at this stage can have significant health benefits beyond improving erectile function.
Psychological Benefits:
Early intervention can also mitigate the psychological impact of ED, including anxiety, depression, and reduced self-esteem. Addressing ED symptoms promptly can help maintain relationship satisfaction and overall quality of life.
Comprehensive Care Approach:
Recognising ED early in diabetic men allows healthcare providers to adopt a more comprehensive care approach, addressing both diabetes and ED together. This holistic management can lead to better health outcomes and improved patient satisfaction.
Diagnosing ED in the Context of Diabetes
Diagnosing erectile dysfunction (ED) in men with diabetes requires a careful and thorough approach. Given the complex interplay between diabetes and ED, the diagnostic process involves a comprehensive evaluation that not only confirms the presence of ED but also identifies underlying diabetic complications that may contribute to the condition.
Initial Medical Consultation:
Patient History:
The process typically begins with a detailed patient history, where the healthcare provider gathers information on the patient’s diabetes management, including duration, medication, and glycemic control levels. Additionally, the patient’s sexual history, including the onset and duration of ED symptoms, is reviewed.
Symptom Assessment:
Specific questions regarding the frequency, quality, and duration of erections, as well as sexual desire and satisfaction levels, help in assessing the severity of ED. Information on lifestyle factors such as smoking, alcohol use, and physical activity is also collected.
Physical Examination
General Health Check:
A physical exam can reveal signs of complications from diabetes that might affect erectile function, including poor circulation, signs of neuropathy, and hormonal imbalances.
Genitourinary Examination:
This focused examination assesses the health of the genitalia and checks for any physical abnormalities that could contribute to ED, such as penile plaques indicative of Peyronie’s disease.
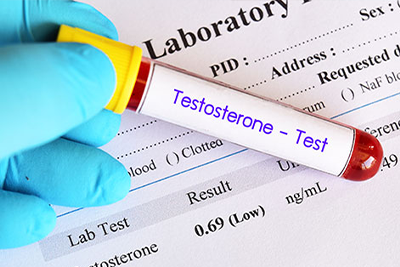
Diagnostic Tests
Blood Tests:
Comprehensive blood tests are conducted to evaluate glucose control (HbA1c levels), lipid profiles, and testosterone levels. These tests help identify diabetes-related factors that may contribute to ED.
Urinalysis:
Urine tests can detect signs of diabetes complications, such as kidney disease, which can also impact erectile function.
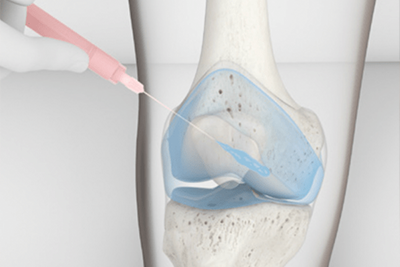
Nocturnal Penile Tumescence (NPT) Test:
The NPT test, which measures erections during sleep, can help differentiate between physical and psychological causes of ED.
Penile Doppler Ultrasound:
This imaging test assesses blood flow to the penis and can identify vascular issues contributing to ED.
Comprehensive Health Evaluation
Identifying Root Causes:
A thorough diagnostic process is essential to identify not just the presence of ED but also underlying diabetic complications or other health issues contributing to the condition.
Personalised Treatment Planning:
Understanding the specific factors contributing to ED in the context of diabetes allows healthcare providers to tailor treatment plans that address both conditions effectively.
Monitoring and Management:
Regular follow-ups and monitoring of diabetes and erectile function are crucial for adjusting treatment plans and ensuring optimal patient outcomes.
ED Treatment Options for Men with Diabetes
Erectile dysfunction (ED) in men with diabetes requires a multifaceted treatment approach that addresses both the symptoms of ED and the underlying diabetic condition. The efficacy of various treatments can vary based on the individual’s specific health profile, including the severity of diabetes and ED.
Pharmacological Treatments
PDE5 Inhibitors:
The first line of treatment often includes phosphodiesterase type 5 (PDE5) inhibitors. These medications enhance erectile function by increasing blood flow to the penis. While effective for many men, diabetic patients may experience variable responses, and adjustments in medication or dosages might be necessary.
Hormonal Therapy:
In cases where low testosterone levels contribute to ED, testosterone replacement therapy may be considered. However, this approach requires careful monitoring, particularly in diabetic men, to manage potential side effects and ensure that testosterone levels are maintained within a safe range.
Other Medications:
For men who do not respond to PDE5 inhibitors, alternative options such as alprostadil (a vasodilator that can be injected into the penis or inserted as a urethral suppository) may be explored. These treatments have shown efficacy in diabetic men with ED, but patient education on proper administration is crucial.
Lifestyle Interventions
Diet and Exercise:
Improving glycemic control through diet and exercise is fundamental for diabetic men with ED. Regular physical activity and a balanced diet not only help manage diabetes but can also improve erectile function by enhancing overall vascular health.
Weight Management:
Achieving and maintaining a healthy weight can significantly impact the management of both diabetes and ED. Weight loss in overweight or obese individuals can improve insulin sensitivity, blood flow, and erectile function.
Smoking Cessation and Limiting Alcohol:
Smoking and excessive alcohol consumption are risk factors for both diabetes and ED. Quitting smoking and moderating alcohol intake can improve cardiovascular health and erectile function.
Surgical Options
Penile Implants:
In cases where pharmacological and lifestyle interventions are not effective, surgical options such as penile implants may be considered. Penile implants, including inflatable and malleable devices, offer a permanent solution to ED but involve a more invasive approach with associated risks.
Efficacy of Treatments and Considerations
Individualised Treatment Plans:
Individual health factors, including the severity of diabetes and the presence of other comorbid conditions, often determine the most effective treatment for ED in diabetic men. A personalised approach, developed in consultation with healthcare providers, is essential.
Monitoring and Adjustments:
Ongoing monitoring of both ED symptoms and diabetes management is crucial for assessing the effectiveness of treatment. Adjustments to treatment plans may be necessary based on response and changes in health status.
Psychological Support:
Addressing the psychological impact of ED and diabetes through counselling or therapy can be an important component of treatment, helping to manage stress, anxiety, and relationship issues that may arise.
Lifestyle Modifications to Improve Diabetes and ED
Lifestyle modifications play a pivotal role in managing both diabetes and erectile dysfunction (ED). Changing daily habits can significantly improve glycemic control, enhance overall health, and positively impact sexual function.
Dietary Adjustments
Heart-Healthy Diet:
Adopting a diet rich in vegetables, fruits, whole grains, lean proteins, and healthy fats can improve cardiovascular health, crucial for managing diabetes and reducing the risk of ED. Limiting processed foods, high sugar, and saturated fats intake is also recommended.
Portion Control and Meal Timing:
Managing portion sizes and eating regularly helps maintain stable blood sugar levels, reducing spikes that can harm vascular health and contribute to ED.
Monitoring Carbohydrate Intake:
Careful monitoring of carbohydrate intake, focusing on complex carbohydrates with a low glycemic index, aids in controlling blood sugar levels, an essential factor for diabetic patients.
Physical Activity
Regular Exercise:
Regular physical activity, such as brisk walking, cycling, or swimming, for at least 150 minutes per week can improve insulin sensitivity, aid in weight management, and boost cardiovascular health, all beneficial for erectile function.
Strength Training:
Incorporating strength training exercises twice a week can enhance muscle mass, leading to better glucose metabolism and improved health outcomes for diabetic individuals.
Flexibility and Balance Exercises:
Practices like yoga and Pilates contribute to physical well-being and reduce stress and anxiety, which can positively affect sexual health.
Smoking Cessation and Limiting Alcohol
Quitting Smoking:
Smoking cessation is critical as smoking exacerbates vascular damage, worsening both diabetes and ED. Resources such as counselling, nicotine replacement therapies, and support groups can aid in quitting.
Moderating Alcohol Consumption:
Reducing alcohol intake can improve overall health and potentially enhance erectile function. Alcohol can interfere with the nervous system and hormone levels, impacting the ability to achieve and maintain an erection.
Impact of Lifestyle Changes
Comprehensive Benefits:
These lifestyle modifications offer comprehensive benefits beyond just improving diabetes and ED. They contribute to weight loss, reduced blood pressure, improved lipid profiles, and enhanced mental health.
Improvement in Glycemic Control:
Better management of blood sugar levels directly impacts the severity and progression of diabetes, reducing the risk of complications that can lead to ED.
Enhanced Sexual Function:
Improved vascular health and stress reduction from lifestyle changes can lead to better erectile function and increased sexual satisfaction.
Psychological Aspects and Support
Dealing with diabetes and erectile dysfunction (ED) concurrently can have profound psychological effects on men, impacting their mental health, self-esteem, and relationships. Understanding the emotional toll of these conditions and exploring avenues for support are crucial steps toward holistic management.
Psychological Impact of Diabetes and ED
Emotional Responses:
Men dealing with both diabetes and ED may experience a range of emotional responses, including frustration, sadness, anxiety, and depression. The loss of sexual function, in particular, can lead to feelings of inadequacy and diminished self-worth.
Impact on Relationships:
ED can strain intimate relationships, leading to communication breakdowns and decreased intimacy. The stress of managing diabetes, coupled with the challenges of ED, can further exacerbate these relationship tensions.
Self-Identity and Masculinity:
For many men, sexual performance is closely tied to notions of masculinity and identity. ED, therefore, can provoke a crisis of self-image, affecting how men perceive themselves and their roles within relationships.
Strategies for Coping
Open Communication:
Encouraging open dialogue with partners about the challenges of diabetes and ED can foster understanding and support, helping to maintain intimacy and strengthen relationships.
Education and Awareness:
Educating oneself about both conditions demystifies them, reducing fear and anxiety. Understanding that these are common issues with viable treatments can be empowering.
Lifestyle Management:
Engaging in lifestyle modifications that improve physical health can also have positive psychological benefits, enhancing overall well-being and self-esteem.
Resources for Psychological Support
Counselling and Therapy:
Professional counselling or therapy can provide valuable support, offering strategies to manage stress, anxiety, and depression. Cognitive-behavioral therapy (CBT), in particular, can be effective in addressing negative thought patterns related to ED and diabetes.
Support Groups:
Joining support groups for men with diabetes and/or ED can offer a sense of community and belonging, reducing feelings of isolation. Sharing experiences and coping strategies with others facing similar challenges can be profoundly reassuring.
Sex Therapy:
For issues specifically related to ED and sexual function, consulting a certified sex therapist can provide targeted strategies to improve sexual confidence and intimacy.
Healthcare Provider Resources:
Many healthcare providers can offer or recommend resources for psychological support, including referrals to mental health professionals specialising in chronic health conditions.
Healthcare Professionals:
Holistic Care Approach:
Healthcare professionals can play a crucial role in identifying the need for psychological support in their patients, adopting a holistic care approach that addresses both the physical and emotional aspects of diabetes and ED.
Referrals and Recommendations:
Physicians should proactively refer patients to mental health services when necessary and recommend supportive resources that can aid in their psychological well-being.
The Healthcare System
For diabetic men facing erectile dysfunction (ED), effectively navigating the healthcare system and communicating with healthcare providers are crucial steps towards receiving appropriate care and support.
Communicating with Healthcare Providers
Preparation:
Before appointments, prepare a list of symptoms, any medications currently being taken, and specific questions or concerns about ED and diabetes management. Being prepared helps ensure that all relevant points are discussed.
Openness and Honesty:
Approach conversations with honesty and openness. Healthcare providers are accustomed to discussing sensitive topics like ED and are there to help, not judge.
Specific Questions:
Ask specific questions about how diabetes may be impacting erectile function, treatment options for ED, and any potential side effects or interactions with current diabetes medications.
Referrals:
Ask for referrals to specialists, such as endocrinologists for diabetes management or urologists for ED treatment, to ensure comprehensive care.
UK Healthcare System
NHS Services:
The National Health Service (NHS) provides a wide range of services for diabetes and ED management. Start with your GP, who can offer initial assessments and refer you to specialists. The NHS also provides counselling and psychological support services for dealing with chronic conditions and their impact on mental health.
Accessing Specialist Care:
Through the NHS, patients can access endocrinologists for diabetes management and urologists for ED treatment. Waiting times can vary, so discussing the expected timelines and any interim support available with your GP is important.
Diabetes Education Programs:
The NHS offers diabetes education programs to help patients better understand and manage their condition. These programs cover diet, exercise, medication management, and monitoring blood sugar levels, all of which can indirectly benefit ED management.
Private Healthcare Options
Vale Health Clinic in Tunbridge Wells:
Private healthcare options like Vale Health Clinic provide an alternative for those seeking more immediate or specialised care. Vale Health Clinic offers personalised treatment plans for ED, including access to the latest therapies and technologies.
Benefits of Private Care:
Private healthcare can offer shorter appointment waiting times and a broader range of treatment options. It also allows for more personalised care and direct access to specialists.
Considerations:
When exploring private healthcare options, consider the costs and whether private health insurance may cover some or all of the services.
Making the Most of Healthcare Services
Integrated Care Approach:
Whether through the NHS or private healthcare, seek an integrated care approach that addresses both diabetes and ED comprehensively. This may involve coordinating care between different specialists and your GP.
Patient Advocacy:
Be an advocate for your health. Don’t hesitate to ask for second opinions, inquire about alternative treatments, or express concerns about your care plan.
In conclusion, diabetes and erectile dysfunction are deeply intertwined, with each condition influencing the other. However, men can effectively manage these conditions with informed management strategies, proactive lifestyle changes, and the support of the healthcare community.
Related Articles
- Erectile Dysfunction and Underlying Health Conditions
- Testing for Erectile Dysfunction Yourself
- Vasectomy and Erectile Dysfunction: The Facts
- Causes of Erectile Dysfunction in the UK
- What Your Testicles Are Telling You